
It’s now been more than a week since our baby Patrick was born. As mentioned in my previous post, we had an unexpected turn of events at the end of what had previously been a very healthy pregnancy.
The whole process was pretty difficult, long (we were in the hospital for almost a week), and emotional; combined with my postpartum hormones and lack of sleep, it took me awhile to fully wrap my head around everything that happened.
I still feel some residual emotion when I look back on that time – it’s little things, like listening to my “soothing” songs playlist, as it reminds me of my stalled labor, and simply wondering if we made the right decision, or what we could have done differently. But ultimately, it feels good to get it all out in the open.
Overall, I’ve realized that with most childbirth experiences, most pregnancies, most initial forays into motherhood, infertility, etc., that each woman likely has her own “cross to bear,” so to speak, and this has been my big one thus far. There’s also an important lesson in the idea that you can plan and plan for something, and life can choose to throw you a major curve ball at the last minute – and you just have to go with it, and learn from the experience.
The Unexpected Turn of Events
Starting in mid-March (a month out from my due date), I had three higher-than-previous blood pressure readings.

In all three cases, the readings were a) still under what’s considered to be a more dangerous reading, and b) were normal upon second reading (i.e. the nurse would take my BP again, and it would be fine). The concern from my OB, however, was that these readings were higher than they had been throughout the rest of my pregnancy, and I was officially diagnosed with gestational hypertension. My due date was a Sunday, and the Tuesday before, it was recommended that my labor be induced.
The reason induction was recommended was because gestational hypertension can lead to preeclampsia, and preeclampsia can come on hard and fast, and is risky for both baby and mom, but especially mom.
There was no guarantee that preeclampsia would happen, and I was definitely in a gray area. And at this point in my pregnancy, I felt great. Like, really great. Very few aches and pains, good energy; I wanted to spend my days before the baby came going on walks, going swimming, hanging out in coffee shops, that sort of thing. As a result, I was crushed and conflicted when induction was recommended, and scheduled for just a few days before my due date.
I cried a lot; I talked it over with family and friends, and ultimately, it all came down to whether it was worth it to risk the health of both the baby and me. As a friend of mine put it (she had done some of her own research when a friend of hers had a similar diagnosis), there would be little to gain and potentially a lot to lose by not going with the recommendation to induce.
I also wrote some questions to the OB who recommended induction (my regular OB was on vacation that particular week, but she had also been leaning towards induction when I saw her the week prior), including a question about whether or not I’d be allowed to walk around and generally be mobile during the induction process. This was especially important to me, so I was relieved when she said yes, and that she thought that was a great idea.
So, we plowed forward. I ran some errands and took a few walks in those last couple of days; Jeffrey and I had a great last “day out” the day before the scheduled induction. We sat on a bench together in Duboce Park in SF, watching dogs and their owners play together, and just soaking in the feeling about everything was about to change. Anticipating a “scheduled” labor is something I didn’t think I’d ever have to experience; while we knew this day was coming, it was so odd to be able to track, minute by minute, when it would (supposedly) arrive.
The Induction Begins – Sort Of

The morning of the induction, Jeffrey and I got up and got breakfast at Brown Sugar Kitchen, which was amazing (so happy we squeezed that in!). We headed back to the house and finished packing up our things. Our induction was scheduled for 12:00pm, but we were advised to call Labor & Delivery beforehand to make sure that they would have room for us when we showed up.
I called at 11:30am, and lo and behold, there was no room. I was asked to call back at 2:00. I called back at 2:00, and was asked to call back at 4:00. In the meantime, I played Donkey Kong Country: Tropical Freeze while Jeffrey half-watched me play, and half-worked on his laptop, and then we took a walk and picked up sandwiches at Berkeley Bowl for dinner.
I called back at 4:00, and there were still no rooms available. Rather than have me keep having to call back, however, the supervising nurse decided instead to have us just show up to the hospital at 9:00pm and start the process in triage (meaning, go over the induction process, take my vitals, take care of paperwork, etc.). We may have still had to just hang out in triage for awhile, but at least we wouldn’t have to keep calling back.

We arrived at 9:00 as planned, and after all that, a room became available just as we arrived. We got all settled in, and we went over the plan for induction. We would start by taking a dose of misoprostol. Then, the baby and I would be monitored for two hours to make sure that we both could tolerate the drug, and if we could, I’d take another dose (and take more if necessary). The drug would then do its thing to ripen my cervix; this could either kickstart labor all on its own, or I’d also take Pitocin (a synthetic version of oxytocin) to help the process along. Either way, it seemed pretty straightforward.
Except it didn’t work. To track the progress, I was outfitted in a hospital gown and an elastic belly band, and two monitors were placed on my belly underneath the belly band (to keep them in place). One monitor tracked the baby’s heart rate, and the other measured whether I was having any contractions. My blood pressure was also taken regularly by my assigned nurse. The OB resident on duty didn’t like the baby’s heart rate on the misoprostol (too many dips), and didn’t want to move forward with another dose (since we wouldn’t be able to un-do an oral medication if it caused additional issues).
They decided to move forward with the Pitocin anyway, to see if that would get my cervix going. At this point, my cervix was a little soft, but not at all dilated. By the way, getting your cervix examined is no picnic. It’s uncomfortable at best and painful at worst, especially when the resident/doctor really has to get their fingers in their to determine the level of dilation.
The First Stage of Pitocin, the First Attempt at a Foley Balloon, and the First Onset of Frustration, Stress, and Tears
To get the Pitocin, I had to be hooked up to an IV. It was Saturday morning at this point. We ordered breakfast through the Kaiser cafeteria (the food wasn’t too bad across the board, actually, and we could order using the TV in our room), and overall, we were still in good spirits. Jeffrey kept friends and family updated on our progress.

The senior OB resident tried inserting a foley balloon, which can help get the cervix going (up to 3-4 centimeters dilated, if successful). However, the cervix basically spat it out as soon as the resident tried inserting it, and she decided to hold off until we had more time on the Pitocin.
As the day went on, the positive energy started depleting. For one, nothing was really progressing. And for another, lying around in bed was getting really uncomfortable and annoying.
I asked if I could start moving around more instead of being bed-ridden. There was a mobile version of the monitor used for the baby’s heart rate and my contractions, so they hooked me up to that, and Jeffrey and I tried taking a walk around the hospital floor carrying the mobile monitor and wires as well as my IV stand. And then we had to stop pretty much as quickly as we began. As it turned out, the mobile monitor didn’t broadcast the signals to the nurses’ station very well, so the nurses couldn’t monitor the baby’s heart rate while I was moving around.
This still didn’t seem too bad; could I sit in our room instead and bounce on the medicine ball that we brought with us? Sure, the nurse said, that should be fine; she even gave me some tips on how to sit on the ball that might encourage labor to start.
And we found ourselves yet again at a loss. After I tried sitting and bouncing for a bit, the baby’s heart rate monitor would shift too much, so the nurse couldn’t get a good read. She came in and asked me to sit still for a minute, and she didn’t like the baby’s overall heart rate, so she asked me to go back to bed and lay down on my side.
Sigh. Back in bed I went. So much for all that wonderful ability to be mobile, a concept I had found so comforting when considering the recommendation to induce.
The day went on, and there was still no progress. At this point, I started getting a little emotional. Our nurse was very sweet and supportive; she encouraged us to talk in detail with the OB residents, and to ask the question of “why are we here?”, and to make sure we’re still doing this for all the right reasons.
The senior OB resident came to check in, and we asked her that question, and also asked her if we could simply stop the induction process and just go home, and see if labor would start on its own. My blood pressure rates had pretty much all been low since I’d checked in, and it seemed like these “forced” efforts were going nowhere.
The OB resident then brought up that the data they’d collected on the baby and me at this point (through all of the monitoring) indicated that my placenta was not performing as well as it should be. If she had to give it a grade, she would give it a C+. The placenta has an expiration date on it, and it looked like mine was perhaps coming to an end a little earlier than they would have wanted. We could have gone home; but then, how would we know if the placenta was giving the necessary support to the baby anymore? And, of course, the risk of preeclampsia was still something to consider.
The Foley Balloon, the Start (and End) of Labor, and the Botched Epidural
Since the Pitocin was a bust, the senior OB resident decided to try the foley balloon again. The upside is that she was able to insert it; the downside is that it was a super unpleasant experience to get it in there. If I never had to have that feeling again, I’d consider myself lucky. But, we got through it.
It was after this that things got pretty interesting, pretty quickly. Jeffrey ran out to get dinner (mac and cheese from Homeroom), and I started having sharp back pain no matter what I did. I actually would get this type of back pain during the third trimester, but it was always linked to me having to pee; as soon as I would go to the bathroom, the pain would go away. This time, however, the pain was just there, and not really going away. The nurse seemed to think that it was the combination of the foley balloon and the position of the baby’s head possibly hitting a nerve in the wrong way.
I put on a movie, and Jeffrey came back with dinner. I tried to eat, but essentially, the pain got too intense. Not only that, but it started coming in the trademark wave-like pattern that indicated I was having contractions.

So, we kicked into “okay, we’re in labor!” mode. I started doing slow, methodical breathing when each contraction came, and Jeffrey supported me and did anything I needed. However, there was something not so typical about these contractions. They quickly got a lot stronger, and would often last about 2 minutes, and would also often be less than 5 minutes apart, and sometimes right on top of each other. These patterns indicated a woman in the later stages of labor – not a woman whose cervix was barely dilated and had just started having contractions.
The OB resident checked, and the foley balloon was in no way ready to budge, which meant my cervix hadn’t yet started to dilate any more than before. So, we could only wait and see. But at that point, I was in a lot of pain, and hadn’t had any sort of “warm-up” to the pain that most women do in labor (i.e., the early labor where contractions aren’t as intense, and there’s more time in between contractions).

I tried nitrous oxide (a pain management solution offered by Kaiser now, which is super cool, as it can be really useful for women in labor and is not yet readily available in many US hospitals; I had been looking forward to trying it out in labor to see if it worked), but it became clear that I would have had to have started it earlier for it to be effective.
Jeffrey and I tried different tactics: I tried sitting on the medicine ball, we tried slow dancing to soft music (I had put together a “soothing” playlist before leaving for the hospital, and it did help), I tried sitting in other positions as well. But my contractions were too intense and too close together.
I was also vomiting heavily during some contractions in particular. The nurses gave me something for the nausea, which helped. It was past midnight at this point, and since this was still considered “early labor,” I knew there was no way I’d be getting any rest, and I still had a long road ahead of me, so I asked for an epidural.
The anesthesiologist arrived and placed the epidural. They told me that it could take some time to set in, so I let that time pass. However, I still wasn’t getting much relief, and I could move my legs around, which seemed strange to me. Another anesthesiologist (somewhat crankily) explained to me that this was normal, that epidurals don’t often help that much with back labor, etc., but that she’d turn mine up a bit, and that I could also hit a button the IV machine to periodically give myself a dose of more relief.
Some additional time passed, and I was actually able to get some sleep, which made me think that the epidural was doing its job. A nurse still needed to come in and help turn me over every hour, so it wasn’t a completely restful night, but it was still better than expected.
In the morning, I pretty much felt fine. I would occasionally get a light contraction wave, but that’s it (and I heard conflicting things from nurses and residents as to whether any contractions were actually being read by the contraction monitor). I wasn’t allowed to get up since the epidural was still placed, and my hips were killing me (the bed was hard, and I could only lay on one hip or the other). This all seemed weird to me — wasn’t an epidural supposed to make me at least somewhat numb from the waist down?
The midwife on duty came in to check in and talk to us, and she checked my cervix, only to find that very little progress had been made (I was maybe 1 centimeter dilated). I started crying out of frustration and exhaustion. The midwife was really great with me, and we discussed all the options, and determined that we would give the foley balloon a little more time to try and do its thing, then we would try misoprostol and Pitocin again in the evening to see how that would go. We also decided to have an anesthesiologist come in and discuss removing my epidural so I could move around a bit, with the idea that I could get another epidural placed again at a later point, if/when my contractions started again.
The anesthesiologist came in, and asked what my level of numbness was, to which I answered: “I’m not numb.” He examined the whole setup, and determined that the epidural had never actually started working. Which essentially meant that the relief I felt overnight was my labor coming to a halt on its own. Which was, once again, super frustrating, but at least I got the botched epidural removed and I could temporarily give my hips some relief.
A Stubborn Cervix, and One Last Attempt to Induce
In the evening, another OB resident came in and removed my foley balloon. This process, thankfully, was far less painful than placing the balloon. After removing, she determined that my cervix was 1.5 centimeters dilated. Still disappointing, of course, but the plan was to try another round of misoprostol, see how the baby and I would handle it, and then administer Pitocin again.
I had a brief break at this point where my assigned nurse unplugged me from everything (save for the IV in my hand) so I could take a shower. It was, quite possibly, one of the best showers I’ve ever taken. It was Sunday, and I hadn’t bathed since Friday; I was stinky, sore, and had crusted blood on my legs from the multiple cervical exams. Needless to say, I felt like a new woman when I was done.
We settled in for the night, and I was given a dose of misoprostol. It was time to wait and see.
Unfortunately, it ended up being a really awful night. The bed felt harder and harder by the minute, and I couldn’t get comfortable no matter how hard I tried (and I normally am not too picky about where I sleep; this definitely wasn’t a “princess and the pea” situation). I asked the nurse for a couple of extra blankets, which I laid down on the bed for some additional cushioning.
Even then, I was woken up frequently. First, the nurse came in and told me that the baby still wasn’t tolerating the misoprostol as well as he should have been, so they weren’t going to administer any more, but that they would still be starting me on Pitocin as planned. So, the IV went in.
I then had to resume the unfortunate pattern of having to unplug myself and drag the IV stand into the bathroom every time I had to pee, which of course was frequently given the fact that I was 40 weeks pregnant. The IV machine was temperamental, and would start beeping loudly throughout the night, and a nurse would have to come in and make an adjustment to get it to stop beeping. The nurse officially assigned to me for that particular shift wasn’t especially pleasant, and at one point turned up the volume on the baby’s monitor for no particular reason, which made it even more difficult to relax and sleep.
At one point, I got up to go to the bathroom, and when trying to plug myself back in to get into bed, got the wires tangled, and the IV machine started beeping again. I was so tired, and I just started sobbing. Jeffrey got up and helped me get untangled and get into bed, and a nurse fixed the machine; but signs were pointing to my emotional state being rather fragile.
All Attempts Have Failed; Only One Option Left
Early in the morning, a nurse came in and told me that the baby’s heart rate was dipping, and that she needed to put me on oxygen. She put on the mask, and the OB resident came in and had them take me off the Pitocin. She informed me that the baby’s heart rate had dipped too many times throughout the night, and that they didn’t want to continue on the Pitocin as a result.
Of course I started crying again; I was just so tired and so overwhelmed. The resident was super sweet, and she told me that she was going to discuss the next steps with the rest of her colleagues and that they’d get back to me ASAP.
I cried for a bit more on Jeffrey’s shoulder, and then just tried to relax. We discussed the concept of the C-section, which we assumed was going to end up being the recommendation at this point, given that nothing else had worked – and if they were still concerned about the state of my placenta, then sending me home didn’t seem to be an option either. We essentially agreed that we were okay with it. It wasn’t what either of us wanted, but we also knew that there didn’t seem to be any better alternatives.
And we were right. The senior OB resident came in to give me an update, and she said that there were two options. One was to break my waters manually, which was considered a last resort, and likely wouldn’t do anything since my cervix wasn’t far enough along (and would increase the risk of bacteria getting to the baby in the meantime). If it did work, it would mean that I would have to start labor over from the beginning, which likely meant a long and arduous process. The other was to move forward with a C-section.
We opted for the the C-section. I knew I was too exhausted to go through the entirety of labor (and that would only be if breaking my waters was actually successful); my body and mind felt wrecked, and I had been bed-ridden for more than 2 days.

So, the C-section was scheduled for the end of the day. The anesthesiologist who would be present for the procedure came in and explained the options for getting me nice and numb (we decided to go with a spinal as opposed to another epidural). My assigned nurse (who had been assigned to me previously, and was super sweet and supportive) gave me the lowdown of how things would go.

She then helped get me unplugged again so that I could take a shower. We also agreed that I would only have to plug into the fetal monitor once an hour for 20 minutes, so I could be mobile for the rest of the time. This made a huge difference – I was able to take some walks around the hallways, walk around my room, sit in a chair or the medicine ball instead of the bed, etc.
Overall, it felt like a major fog had been lifted. While I didn’t set out to choose a C-section, just knowing that there was an end in sight, and that we were in good hands, was a huge relief.
The C-Section, and the Magic of Disney Songs

One of the biggest thing that I worried about with a C-section (besides the post-procedure recovery and other surgery-related risks) was the fact that while I would be completely numb from the breast down, I would still feel a fair amount of tugging and/or pressure. I didn’t look forward to this feeling, and if it would make me anxious/panicky in the moment. Jeffrey and I discussed ways to help me relax, and we decided it might be fun to sing Disney songs together.
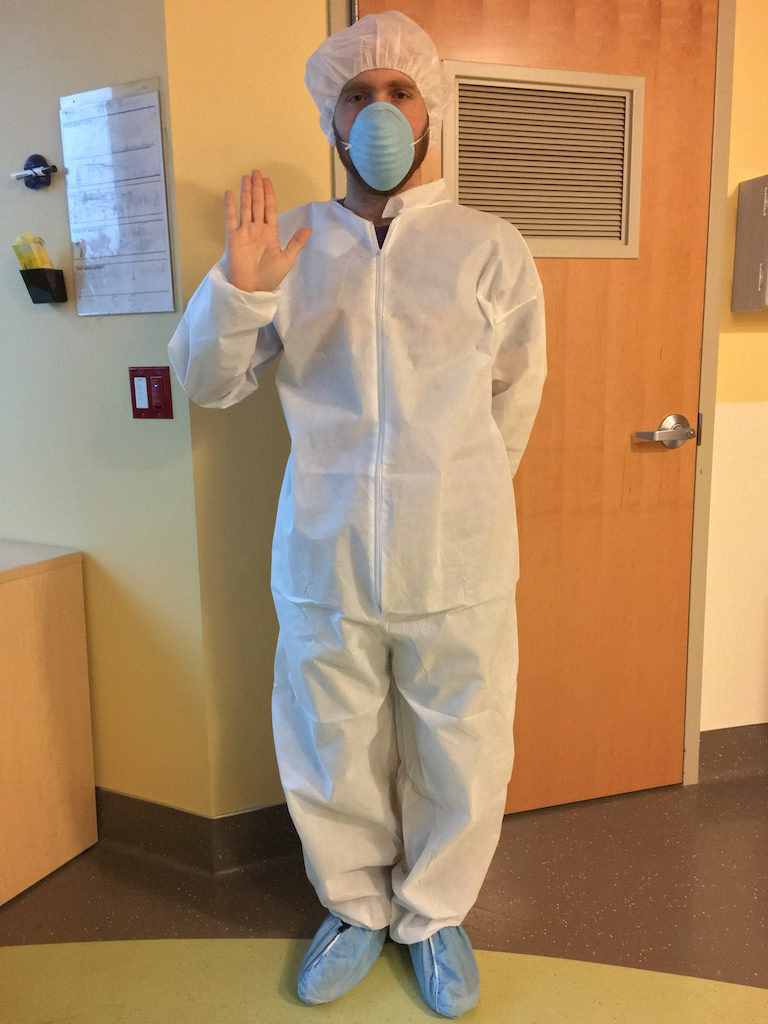
When it was time, we were led down the hall, and Jeffrey waited behind while I was prepped. I met the whole team, who were really awesome and friendly and did everything they could to make me feel comfortable. One woman in particular just sat and talked with me while we waited for the anesthesiologist.
The OB resident and supervising OB asked if I had any requests for music to be played during the procedure, and we discussed some options, but I also mentioned the plan that Jeffrey and I had to sing Disney songs to each other, so they put on a Disney Pandora station, which was really cute.
It was pretty strange to be completely numb from the breast down. For a minute or two while the numbness was fully setting in, I kept having the urge to move my legs, but I couldn’t. I also had to make sure to focus on my breathing, as it was easy to feel like I wasn’t breathing (the anesthesiologist warned me about this particular feeling). It was easy to get used to, however.

And then, I was all set. Jeffrey came in, and I can’t quite describe the emotions I was feeling – I was basically all over the map. Jeffrey was wonderful; he held my hand and started singing along to “I Just Can’t Wait to Be King,” which was what was playing on the Pandora station.
And then, before we could even fully process what has happening, and before the song was even over, I felt one big tug (I said, “I feel like I can’t breathe!”), and then the surgical team said “He’s out!” And he was! It was so fast! Jeffrey was brought over the warming table to be with the baby while the baby nurse did her thing (the Apgar score, etc.).

The anesthesiologist was really great with me – he talked to me gently while the baby was being evaluated, explaining what they were looking for, that sort of thing. And then, they brought Patrick over to do some skin-to-skin on my chest. It was a little more awkward than I imagine it would have been for a vaginal birth – my head and chest were at a bit of a downward slope behind the big drape, so I couldn’t see him super well while he was on my chest, but regardless, it was that magical moment that everyone talks about.
In fact, for me, the magical moment really did start as soon as they got him out and said “he’s out!”. I immediately felt myself get choked up, and this overwhelming feeling of love just washed over me. I think it did for Jeffrey too – he was so excited to see him, and he got some great initial photos and videos of Patrick and me, post-procedure.

We were then wheeled down to another room for an hour and a half or so of recovery. A couple of nurses took good care of me (taking my vitals, giving me fluids, etc.) as well as the baby. Patrick was able to do the initial breastfeed – he actually latched on right away, which was very encouraging.
The Aftermath and Recovery
The next few days were spent in the maternity wing of the hospital, on the same floor as Labor & Delivery. It became apparent early on that my recovery was going to be faster than usual – I was able to initially get out of bed quite easily (without having dizziness or other surgery-related difficulties when trying to move), I urinated quickly and easily after the catheter was removed, I was able to sit up in bed with little assistance, etc. This was super encouraging, as I had been dreading a long and difficult recovery following such major surgery.

Myself and the baby were monitored during this time to make sure everything was okay, and all was well. We also got a nice little crash course in caring for a newborn (something we’re still learning, of course). The silver lining of us having to spend extra days in the hospital is that we got more time with the nursing staff at Kaiser. All of the staff work with babies all day, and many of them have kids of their own, so they were all happy to give their own tips on breastfeeding, getting the baby to rest, etc.

In general, while this whole process wasn’t what we wanted or planned for, I can’t say enough good things about the staff at Kaiser, and how we were treated. Almost every single nurse, doctor, staff person, etc. that we encountered was so nice and supportive, and I’m grateful that we had such a solid support system throughout the process.
Now we’re at home, and Patrick is 11 days old as of this post. We still have a lot to learn, and this is a tough period all on its own (No sleep! All he does is eat! So many diapers! My poor nipples!), but overall, we’re doing pretty well – just adjusting to our new life. The days feel both long and short at the same time; but of course, everyone keeps saying how fast it will go by, so there’s that.
I hardly feel any pain or discomfort anymore from the surgery, and I try to go on walks every day, so that’s felt great. I’m looking forward to when I can work out again, when I can take longer/faster walks, etc.
All in all, I can’t say that I don’t somewhat regret the decision to induce. However, this isn’t an “active” sense of regret – instead, it’s more of a feeling of “if I could do this again, maybe I would have done something different.” But this is what happened, and we can’t take it back, and most importantly, both Patrick and I are healthy and happy. In this case, it wasn’t about the journey, but the destination.